|
References
SECTION ONE: Introduction
Alanis, A. J. 2005. Resistance to antibiotics: are we in the post-antibiotic era? Archives of Medical Research 36:697–705.
Awad, A. I., D. E. Ball, and I. B. Eltayeb. 2007. Improving rational drug use in Africa: the example of Sudan. Eastern Mediterranean Health Journal 13:1202–11.
Berild, D., T. G. Abrahamsen, S. Andresen, et al. 2008. A controlled intervention study to improve antibiotic use in a Russian pediatric hospital. International Journal of Antimicrobial Agents 31:478–83.
Higashi, T., and S. Furuhara. 2009. Antibiotic prescriptions for upper respiratory tract infection in Japan. Internal Medicine 48:1369–75.
Isturiz, R. E., and C. Carbon. 2000. Antibiotic use in developing countries. Infection Control and Hospital Epidemiology 21:394–7.
Kaier, K., C. Wilson, M. Chalkley, et al. 2008. Health and economic impacts of antibiotic resistance in European hospitals—outlook on the BURDEN project. Infection 36):492–4.
Khor, M. 2005. TWN Info Service on Health Issues No. 9: Irrational drug use causing rise of antimicrobial resistance. Third World Network. http://www.twnside.org.sg/title2/health.info/twninfohealth009.htm.
Meropol, S. B., Z. Chen, and J. P. Metlay. 2009. Reduced antibiotic prescribing for acute respiratory infection in adults and children. British Journal of General Practice 59:e321–8.
Monnet D. L., and K. G. Kristinsson. 2008. Turning the tide of antimicrobial resistance: Europe shows the way. Eurosurveillance 13:19039.
Pharmaceutical Security Institute. 2011. Counterfeit Situation. http://www.psi-inc.org/counterfeitSituation.cfm.
PRWeb. 2011. Global antibiotics market to reach US$40.3 billion by 2015, according to new report by Global Industry Analysts, Inc., news release, October 25. http://www.prweb.com/releases/antibiotics/anti_infectives/prweb4688824.htm.
Russell, A. D. 1997. Plasmids and bacterial resistance to biocides. Journal of Applied Microbiology 83:155–65.
Tucker, M. E. 2010. Cost of antibiotic resistance hits private payers. Hospitalist News (March 1). http://www.ehospitalistnews.com/specialty-focus/infectious-diseases/single-article-page/
cost-of-antibiotic-resistance-hits-private-payers/6031fbf760.html.
Tünger, O., G. Dinç, B. Ozbakkaloglu, U. C. Atman, and U. Algün. 2000. Evaluation of rational antibiotic use. International Journal of Antimicrobial Agents 15:131–5.
Weinstein, R. A. 2001. Controlling antimicrobial resistance in hospitals: infection control and use of antibiotics. Emerging Infectious Diseases 7:188–92.
Woodward, R. S., G. Medoff, M. D. Smith, and J. L. Gray. 1987. Antibiotic cost savings from formulary restrictions and physician monitoring in a medical-school-affiliated hospital. American Journal of Medicine 83:817–23.
World Health Organization. 2011. Combat antibiotic resistance. http://whd2011.euro.who.int.
|
|
World Health Organization. 2011. World Health Day 2011. Combat drug resistance: no action today means no cure tomorrow. Statement by WHO Director-General, Dr Margaret Chan, http://www.who.int/mediacentre/news/statements/2011/whd_20110407/en./index.html.
World Health Organization. 2010. Medicines: rational use of medicines. http://www.who.int/mediacentre/factsheets/fs338/en/index.html.
World Medical Association. 2011. WMA Statement on Resistance to Antimicrobial Drugs. http://www.wma.net/en/30publications/10policies/a19/index.html.
SECTION TWO. Understanding AMDR: The Knowledge Base
Abu-Raddad, L. J., P. Patnaik, and J. G. Kublin. 2006. Dual infection with HIV and malaria fuels the spread of both diseases in sub-Saharan Africa. Science 314:1603–6.
Adjuik, M., A. Babiker, P. Garner, P. Olliaro, W. Taylor, N. White, and the International Artemisinin Study Group. 2004. Artesunate combinations for treatment of malaria: meta-analysis. Lancet 363:9–17.
Aguiar, F., M. A. Vieira, A. Staviack, et al. 2009. Prevalence of anti-tuberculosis drug resistance in an hiv/aids reference hospital in Rio de Janeiro, Brazil. International Journal of Tuberculosis and Lung Diseases 13:54–61.
Akwar, H. T., C. Poppe, J. Wilson, et al. 2008. Associations of antimicrobial uses with antimicrobial resistance of fecal Escherichia coli from pigs on 47 farrow-to-finish farms in Ontario and British Columbia. Canadian Journal of Veterinary Research 72:202–10.
Ammerlaan, H., H. Seifert, S. Harbarth, et al. 2009. Adequacy of antimicrobial treatment and outcome of Staphylococcus aureus bacteremia in 9 Western European countries. Clinical Infectious Diseases 49:1006–8.
Ananthakrishnan, A .N. 2011. Clostridium difficile infection: epidemiology, risk factors and management. National Reviews of Gastroenterology and Hepatology 8:17–26.
Aquirre-Avalos, G., J. C. Mijangos-Méndez, and G. Amaya-Tapia. 2010. Acinetobacter baumannii bacteremia. Revista Medica del Instituto Mexicano del Seguro Social 48:625–34.
Baird, J. W. 1997. Antibiotic prescribing, controls, and antimicrobial resistance: an Australian experience. Alliance for the Prudent Use of Antibiotic Newsletter 15:1–2,6.
Barraclough, K. A., C. M. Hawley, E. G. Playford, and D. W. Johnson. 2009. Prevention of access-related infection in dialysis. Expert Review of Anti-Infective Therapy. 7:1185–200.
Berkowtiz, F. E. 1995. Antibiotic resistance in bacteria. Southern Medical Journal 88:797–804.
Blot, S. I., K. H. Vandewoude, E. A. Hoste, and F. A. Colardyn. 2002. Outcome and attributable mortality in critically ill patients with bacteremia involving methicillin-susceptible and methicillin-resistant Staphylococcus aureus. Archives of Internal Medicine 162: 2229–35.
Boucher, H. W., G. H. Talbot, J. S. Bradley, et al. 2009. Bad bugs, no drugs: no ESKAPE! An update from the Infectious Diseases Society of America. Clinical Infectious Diseases 48:1–12.
Breman, J. G. 2009. Eradicating malaria. Science Progress 92(Pt 1):1–38.
|
|
Bright, R. A., D. K. Shay, B. Shu, N. J. Cox, and A. J. Klimov. 2006. Adamantane resistance among influenza A viruses isolated early during the 2005-2006 influenza season in the United States. Journal of the American Medical Association 295:891–4.
Centers for Disease Control and Prevention. 2008. Surveillance for community-associated Clostridium difficile --- Connecticut, 2006. Morbidity and Mortality Weekly Report 57:340–3.
Centers for Disease Control and Prevention. 2009. Update: influenza activity --- United States, August 30--October 31, 2009. Morbidity and Mortality Weekly Report 58:1236–41.
Centers for Disease Control and Prevention. 2010. Influenza antiviral drug resistance: questions and answers. http://www.cdc.gov/flu/about/qa/antiviralresistance.htm.
Centers for Disease Control and Prevention. 2011. Investigation announcement: outbreak of Shiga toxin-producing E. coli O104 (STEC O104:H4) infections associated with travel to Germany. http://www.cdc.gov/ecoli/2011/ecoliO104.
Chan, K. S., M. L. Ling, L. Y. Hsu, and A. L. Tan. 2009. Methicillin-resistant Staphylococcus aureus throat colonization among healthcare workers during an outbreak in Singapore General Hospital. Infection Control and Hospital Epidemiology 30:95–6.
Chang, H. L., C. H. Tang, Y. M. Hsu, et al. 2009. Nosocomial outbreak of infection with multi-drug resistant Acinetobacter baumannii in a medical center in Taiwan. Infection Control and Hospital Epidemiology 30:34–8.
Chang, S., A. K. Sethi, B. C. Eckstein, U. Stiefel, J. L. Cadnum, and C. J. Donskey. 2009. Skin and environmental contamination with methicillin-resistant Staphylococcus aureus among carriers identified clinically versus through active surveillance. Clinical Infectious Diseases 48:1423–28.
Chapin, A., A. Rule, K. Gibson, T. Buckley, and K. Schwab. 2005. Airborne multidrug-resistant bacteria isolated from a concentrated swine feeding operation. Environmental Health Perspectives 113:137–42.
Charlebois, E. D., F. Perdreau-Remington, B. Kreiswirth, et al. 2004. Origins of community strains of methicillin-resistant Staphylococcus aureus. Clinical Infectious Diseases 39:47–54.
Choi, S., J. E. Lee, S. J. Park, et al. 2008. Emergence of antibiotic resistance during therapy for infections caused by Enterobacteriaceae producing AmpC β-lactamase: implications for antibiotic use. Antimicrobial Agents and Chemotherapy 52:995–1000.
Church, J. D., S. B. Omer, L. A. Guay, et al. 2008. Analysis of nevirapine (NVP) resistance in Ugandan infants who were HIV infected despite receiving single-dose (SD) NVP versus SD NVP Plus Daily NVP up to 6 weeks of age to prevent HIV vertical transmission. The Journal of Infectious Diseases 198:1075–82.
Cohen, F. L., and D. Tartasky. 1997. Microbial resistance to drug therapy: a review. American Journal of Infection Control 25:51–64.
Cosgrove, S. E. 2006. The relationship between antimicrobial resistance and patient outcomes: mortality, length of hospital stay, and health care costs. Clinical Infectious Diseases 42(suppl 2):S82–9.
Cosgrove, S. E., G. Sakoulas, E. N. Perencevich, M. J. Schwaber, A. W. Karchmer, and Y. Carmeli. 2003. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clinical Infectious Diseases 36:53–9.
|
|
Costelloe, C., C. Metcalfe, A. Lovering, D. Mant, and A.D. Hay. 2010. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ 340:c2096.
Creel, A. M., S. H. Durham, K. W. Benner, J. A. Allen, and M. K. Winkler. 2009. Severe invasive community-associated methicillin-resistant Staphylococcus aureus infections in previously healthy children. Pediatric Critical Care 10:405–7.
Curry, S. R., J. W. Marsh, K. A. Shutt, et al. 2009. High frequency of rifampin resistance identified in an epidemic Clostridium difficile clone from a large teaching hospital. Clinical Infectious Diseases 48:425–9.
D'Agata, E. M., G. F. Webb, M. A. Horn, R. C. Moellering Jr, and S. Ruan. 2009. Modeling the invasion of community-acquired methicillin-resistant Staphylococcus aureus into hospitals. Clinical Infectious Diseases 48:274–84.
Diaz-Granados, C. A., S. M. Zimmer, M. Klein, and J. A. Jernigan. 2005. Comparison of mortality associated with vancomycin-resistant and vancomycin-susceptible enterococcal bloodstream infections: a meta-analysis. Clinical Infectious Diseases 41:327–33.
Diene, S. M., N. Bruder, D. Raoult, and J. M. Rolain. 2011. Real-time PCR assay allows detection of the New Dehli metallo-β-lactamase (NDM-1)-encoding gene in France. International Journal of Antimicrobial Agents 37:544–6.
Dondorp, A. M., P. N. Newton, M. Mayxay, et al. 2004. Fake antimalarials in Southeast Asia are a major impediment to malaria control: multinationalcross-sectional survey on the prevalence of fake antimalarials. Tropical Medicine and International Health 9:1241–46.
DuPont, H. L., C. D. Ericsson, M. J. Farthing, et al. 2009. Expert review of the evidence base for prevention of travelers’ diarrhea. Journal of Travel Medicine 16:149–60.
Fridkin, S.K., J.C. Hageman, M. Morrison et al. 2005. Methicillin resistant Staphylococcus aureus disease in three communities. New England Journal of Medicine 352:1436–44.
Gandara, A., L. C. Mota, C. Flores, H. R. Perez, C. F. Green, and S. G. Gibbs. 2006. Isolation of Staphylococcus aureus and antibiotic-resistant Staphylococcus aureus from residential indoor bioaerosols. Environmental Health Perspectives 114:1859–64.
Gandhi, N. R., A. Moll, A. W. Sturm, et al. 2006. Extensively drug-resistant tuberculosis as a cause of death in patients co-infected with tuberculosis and HIV in a rural area of South Africa. Lancet 368:1575–80.
García-Álvarez, L., M. T. Holden, H. Lindsay, et al. 2011. Meticillin-resistant Staphylococcus aureus with a novel mecA homologue in human and bovine populations in the UK and Denmark: a descriptive study. Lancet Infectious Diseases 11:595-603.
Gaspari, R. J., E. Dickson, J. Karlowsky, and G. Doern. 2006. Multidrug resistance in pediatric urinary tract infections. Microbial Drug Resistance 12:126–29.
Giske, C. G., D. L. Monnet, O. Cars, Y. Carmeli, and ReAct-Action on Antibiotic Resistance. 2008. Clinical and economic impact of common multidrug-resistant gram-negative bacilli. Antimicrobial Agents and Chemotherapy 52:813–21.
|
|
Glikman, D., Z. Zonis, M. Hindiyeh, et al. 2010. Development of oseltamivir resistance during oseltamivir therapy in a child with severe 2009 H1N1 influenza. Pediatric Infectious Disease 29:385–6.
Gooskens, J., M. Jonges, E. C. Claas, A. Meijer, and A. C. Kroes. 2009. Prolonged influenza virus infection during lymphocytopenia and frequent detection of drug-resistant virus. The Journal of Infectious Diseases 199:1435–41.
Gordon, D.F., and J. C. Gannon. 2000. The global infectious disease threat and its implications for the United States. National Intelligence Council. http://www.dni.gov/nic/special_globalinfectious.html.
Grundmann, H., D. M. Aanensen, C. C. van den Wijngaard, B. G. Spratt, D. Harmsen, A. W. Friedrich, and the European Staphylococcal Reference Laboratory Working Group. 2010. Geographic distribution of Staphylococcus aureus causing invasive infections in Europe: a molecular-epidemiological analysis. PLoS Medicine 7:e1000215.
Gulbinovic, J., K. E. Myrbäck, J. Bytautiene, B. Wettermark, J. Struwe, and U. Bergman. 2001. Marked differences in antibiotic use and resistance between university hospitals in Vilnius, Lithuania, and Huddinge, Sweden. Microbial Drug Resistance 7:383–9.
Hicks, L. A., Y-W Chien, T. H. Taylor, M. Haber, and K. P. Klugman. 2011. Outpatient antibiotic prescribing and non-susceptible Streptococcus pneumoniae in the United States, 1996–2003. Clinical Infectious Diseases 53:631–39.
Hicks, L. A., L.H. Harrison, B. Flannery, et al. 2007. Incidence of pneumococcal disease due to non–pneumococcal conjugate vaccine (PCV7) serotypes in the United States during the era of widespread PCV7 vaccination, 1998–2004. Journal of Infectious Diseases 196:1346–54.
Holmberg, S. D., S. L. Solomon, and P. A. Blake. 1987. Health and economic impacts of antimicrobial resistance. Reviews of Infectious Diseases 9:1065–78.
Hota, S., Z. Hirji, K. Stockton, et al. 2009. Outbreak of multidrug-resistant Pseudomonas aeruginosa colonization and infection secondary to imperfect intensive care unit room design. Infection Control and Hospital Epidemiology 30:25–33.
Howard, D. H. 2004. Resistance-induced antibiotic substitution. Health Economics 13:585–95.
Hsu J., C. Abad, M. Dinh, and N. Safdar. 2010. Prevention of endemic healthcare-associated Clostridium difficile infection: reviewing the evidence. American Journal of Gastroenterology 105:2327–39.
Huycke, M. M., D. F. Sahm, and M. S. Gilmore. 1998. Multiple-drug resistant enterococci: the nature of the problem and an agenda for the future. Emerging Infectious Diseases 4:239–49.
Jenkins, S. G., S. D. Brown, and D. J. Farrell. 2008. Trends in antibacterial resistance among Streptococcus pneumoniae isolated in the USA: update from PROTEKT US Years 1-4. Annals of Clinical Microbiology and Antimicrobials 7:1.
Johnson, L. B., J. Jose, F. Yousif, J. Pawlak, and L. D. Saravolatz. 2009. Prevalence of colonization with community-acquired methicillin-resistant Staphylococcus aureus among end-stage renal disease patients and healthcare workers. Infection Control and Hospital Epidemiology 30:4–12.
Kelesidis, T., I. Kelesidis, P. I. Rafailidis, and M. E. Falagas. 2007. Counterfeit or substandard antimicrobial drugs: a review of the scientific evidence. Journal of Antimicrobial Chemotherapy 60:214–36.
|
|
Kelly, C. P., and J. T. LaMont. 2008. Clostridium difficile—more difficult than ever. The New England Journal of Medicine 359:1932–40.
Klevens, R. M., J. R. Edwards, F. C. Tenover, L. C. McDonald, T. Horan, R. Gaynes, and the National Nosocomial Infections Surveillance System. 2006. Changes in the epidemiology of methicillin-resistant Staphylococcus aureus in intensive care units in US hospitals, 1992-2003. Clinical Infectious Diseases 42: 389–91.
Klevens, R. M., M. A. Morrison, J. Nadle, et al. 2007. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. Journal of the American Medical Assocation 298:1763–71.
Kollef, M. H., L. M. Napolitano, J. S. Solomkin, et al. 2008. Health care-associated infection (HAI): a critical appraisal of the emerging threat-proceedings of the HAI Summit. Clinical Infectious Diseases 47(suppl 2):S55–99; quiz S100–1.
Kouanfack, C., C. Montavon, C. Laurent, et al. 2009. Low levels of antiretroviral-resistant HIV infection in a routine clinic in Cameroon that uses the World Health Organization (WHO) public health approach to monitor antiretroviral treatment and adequacy with the WHO recommendation for second-line treatment. Clinical Infectious Diseases 48:1318–22.
Kuehnert, M. J., H. A. Hill, B. A. Kupronis, J. I. Tokars, S. L. Solomon, and D. B. Jernigan. 2005. Methicillin-resistant-Staphylococcus aureus hospitalizations, United States. Emerging Infectious Diseases 11:868–72.
Kuehnert, M. J., D. Kruszon-Moran, H. A. Hill, et al. 2006. Prevalence of Staphylococcus aureus nasal colonization in the United States, 2001-2002. The Journal of Infectious Diseases 193:172–9.
Laxminarayan, R. 2001. Fighting antibiotic resistance: can economic incentives play a role? Resources 143:9–12.
Lee, K. S., P. C. Divis, S. K. Zakaria, et al. 2011. Plasmodium knowlesi: reservoir hosts and tracking the emergence in humans and macaques. PLoS Pathogens; 7:e1002015.
Lei, T., W. Tian. L. He, et al. 2010. Antimicrobial resistance in Escherichia coli isolates from food animals, animal food products and companion animals in China. Veterinary Microbiology 146:85–9.
Levy, S. B. 1993. Confronting multidrug resistance: a role for each of us. Journal of the American Medical Association 269:1840–2.
Lin, C. C., J. L. Wang, C. Y. Lin, et al. 2009. Methicillin-resistant Staphylococcus aureus bacteremia in patients with end-stage renal disease in Taiwan: distinguishing between community-associated and healthcare-associated strains. Infection Control and Hospital Epidemiology 30:89–92.
Little, S. J., S. Holte, J. P. Routy, et al. 2002. Antiretroviral-drug resistance among patients recently infected with HIV. The New England Journal of Medicine 347:385–94.
Liu, C., A. Bayer, S. E. Cosgrove, et al. 2011. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clinical Infectious Diseases 52:285–92.
Livermore, D. M. 2003. Bacterial resistance: origins, epidemiology, and impact. Clinical Infectious Diseases 36(suppl 1):S11–23.
|
|
Livermore, D. M., and A. Pearson. 2007. Antibiotic resistance: location, location, location. Clinical Microbiology and Infection 13(suppl 2):7–16.
Llor, C., and J. M. Cots. 2009. The sale of antibiotics without prescription in pharmacies in Catalonia, Spain. Clinical Infectious Diseases 48:1345–9.
LoBue, P. 2009. Extensively drug-resistant tuberculosis. Current Opinion in Infectious Diseases 22:167–73.
Long, R., H. Chong, V. Hoeppner, et al. 2009. Empirical treatment of community-acquired pneumonia and the development of fluoroquinolone-resistant tuberculosis. Clinical Infectious Diseases 48:1354–60.
Lowy, F. D. 2010. Mapping the distribution of invasive Staphylococcus aureus across Europe. PloS Medicine 7:e1000215.
Mainous, A. G., III, C. J. Everett, R. E. Post, V. A. Diaz, and W. J. Hueston. 2009. Availability of antibiotics for purchase without a prescription on the internet. Annals of Family Medicine 7:431–35.
Mangione-Smith, R., E. A. McGlynn, M. N. Elliott, L. McDonald, C. E. Franz, and R. L. Kravitz. 2001. Parent expectations for antibiotics, physician-parent communication, and satisfaction. Archives of Pediatrics & Adolescent Medicine 155:800–6.
Masquelier, B., K. Bhaskaran, D. Pillay, et al. 2005. Prevalence of transmitted HIV-1 drug resistance and the role of resistance algorithims: data from seroconverters in the CASCADE collaboration from 1987 to 2003. Journal of Acquired Immune Deficiency Syndromes 40:505–11.
Memoli, M. J., R. J. Hrabal, A. Hassantoufighi, et al. 2010. Rapid selection of a transmissible multidrug- resistant influenza A/H3N2 virus in an immunocompromised host. The Journal of Infectious Diseases 201:1397–403.
Meyers, B. R. 1987. Bacterial resistance: exploring the facts and myths. Bulletin of the New York Academy of Medicine 63:211–6.
Mokaddas, E. M., V. O. Rotimi, and M. J. Albert. 2007. Increasing prevalence of antimicrobial resistance in Streptococcus pneumoniae in Kuwait: implications for therapy. Microbial Drug Resistance 13:227–34.
Murray, R. J., J. O. Robinson, J. N. White, et al. 2010. Community-acquired pneumonia due to pandemic A(H1N1)2009 influenzavirus and methicillin resistant Staphylococcus aureus co-infection. PLoS One 5:e8705.
Naber, C. K. 2009. Staphylococcus aureus bacteremia: epidemiology, pathophysiology, and management strategies. Clinical Infectious Diseases 48(suppl 4):S231–37.
Nicogossian, A., N. Ebadirad, T. Zimmerman, G. Kreps, and E. J. Septimus. 2010. Influenza immunization: synthesizing and communicating the evidence. World Medical and Health Policy DOI: 10.2202/1948-4682.1090.
Nylund, C. M., A. Goudie, J. M. Garza, G. Fairbrother, and M. B. Cohen. 2011. Clostridium difficile infection in hospitalized children in the United States. Archives of Pediatrics & Adolescent Medicine 165:451–7.
O'Fallon, E., S. Gautam, and E. M. D’Agata. 2009. Colonization with multidrug-rresistant gram-negative bacteria: prolonged duration and frequent cocolonization. Clinical Infectious Diseases 48:1375–81.
|
|
Oie, S., A. Obayashi, H. Yamasaki, et al. 2011. Disinfection methods for spores of Bacillus atrophaeus, B. anthracis, Clostridium tetani, C. botulinum and C. difficile. Biological and Pharmaceutical Bulletin 34:1325–9.
Palacios E., R. Dallman, M. Muñoz, et al. 2009. Drug-resistant tuberculosis and pregnancy: treatment outcomes of 38 cases in Lima, Peru. Clinical Infectious Diseases 48:1413–9.
Pallecchi, L., C. Lucchetti, A. Bartoloni, et al. 2007. Population structure and resistance genes in antibiotic-resistant bacteria from a remote community with minimal antibiotic exposure. Antimicrobial Agents and Chemotherapy 51:1179–84.
Pedal, I., and O. Nolte. 2010. Community-associated MRSA and Panton-Valentine leukocidin (PVL): novel trends in epidemiology and forensic implications. Archiv fur Kriminologie 225:119–29.
Peleg, A. Y., D. Monga, S. Pillai, E. Mylonakis, R. C. Moellering Jr, and G. M. Eliopoulos. 2009. Reduced susceptibility to vancomycin influences pathogenicity in Staphylococcus aureus infection. The Journal of Infectious Diseases 199:532–6.
Pongtavornpinyo, W., S. Yeung, I. M. Hastings, A. M. Dondorp, N. P. Day, and N. J. White. 2008. Spread of anti-malarial drug resistance: mathematical model with implications for ACT drug policies. Malaria Journal 7:229.
Powers, J. H. 2009. Risk perception and inappropriate antimicrobial use: yes, it can hurt. Clinical Infectious Diseases 48:1350–53.
Richman, D. D., S. C. Morton, T. Wrin, et al. 2004. The prevalence of antiretroviral drug resistance in the United States. AIDS 18:1393–1401.
Riley, T. V. 1988. Antimicrobial resistance in Branhamella catarrhalis. The Journal of Antimicrobial Chemotherapy 21:147–50.
Robert Koch Institute (RKI). 2011. New epidemiological data support current dietary recommendations of BfR: Joint press release of Federal Institute for Risk Assessment (BfR)/ Robert Koch Institute (RKI). http://www.rki.de/cln_178/nn_217400/EN/Home/PM__072011.html.
Robicsek, A., J. L. Beaumont, and L. R. Peterson. 2009. Duration of colonization with methicillin-resistant Staphylococcus aureus. Clinical Infectious Diseases 48:910–3.
Rosen, J. B., A. R. Thomas, C. A. Lexau, et al. 2011. Geographic variation in invasive pneumococcal disease following pneumococcal conjugate vaccine introduction in the United States. Clinical Infectious Diseases. 53:137–43.
Rosengren, L. B., C. L. Waldner, R. J. Reid-Smith, S. L. Checkley, M. E. McFall, and A. Rajic. 2008. Antimicrobial resistance of fecal Escherichia coli isolated from grow-finish pigs in 20 herds in Alberta and Saskatchewan. Canadian Journal of Veterinary Research 72:160–7.
Ruppé, E., S. Hem, S. Lath, et al. 2009. CTX-M β-lactamases in Escherichia coli from community-acquired urinary tract infections, Cambodia. Emerging Infectious Diseases 15:741–8.
Russell, A. D. 1999. Bacterial resistance to disinfectants: present knowledge and future problems. The Journal of Hospital Infection 43(suppl):S57–68.
Saha, S. K., A. Naheed, S. El Arifeen, et al. 2009. Surveillance for invasive Streptococcus pneumoniae disease among hospitalized children in Bangladesh: antimicrobial susceptibility and serotype distribution. Clinical Infectious Diseases 48(suppl 2):S75–81.
|
|
Savona, N. 2010. Older people are at risk of sexually transmitted infections. Sexually Transmitted Infections 87:70.
Schentag, J. J. 1995. Understanding and managing microbial resistance in institutional settings. American Journal of Health-System Pharmacy 52(6 suppl 2):S9–14).
Schlagenhauf-Lawlor, P. Travelers' Malaria. Ontario: BC Decker Inc, 2008.
Scott, P., E. Arnold, B. Evans, et al. 2004. Surveillance of HIV antiretroviral drug resistance in treated individuals in England: 1998-2000. The Journal of Antimicrobial Chemotherapy 53:469–73.
Sethi, A. K, W. N. Al-Nassir, M. M. Nerandzic, and C. J. Donskey. 2009. skin and environmental contamination with vancomycin-rresistant enterococci in patients receiving oral metronidazole or oral vancomycin treatment for Clostridium difficile-associated disease. Infection Control and Hospital Epidemiology 3:13–24.
Shakoor, O., R. B. Taylor, and R. H. Behrens. 1997. Assessment of the incidence of substandard drugs in developing countries. Tropical Medicine and International Health 2:839-45.
Small, P. M., R. W. Shafer, P. C. Hopewell, et al. 1993. Exogenous reinfection with multidrug-resistant Mycobacterium tuberculosis in patients with advanced HIV infection. The New England Journal of Medicine 328:1137–44.
Smith, R. D., and J. Coast. 2002. Antimicrobial resistance: a global response. Bulletin of the World Health Organization 80:126–33.
Smith, T. C., and N. Pearson. 2011. The emergence of Staphylococcus aureus ST398. Vector Borne and Zoonotic Diseases. 11:327–39.
Standing Medical Advisory Committee Sub-group on Antimicrobial Resistance. 1998. The Path of Least Resistance: Main Report. United Kingdom Department of Health. http://www.advisorybodies.doh.gov.uk/pub/docs/doh/smacrep.pdf.
Targett, G. A. T., ed. Malaria: Waiting for the Vaccine. New York: John Wiley and Sons, 1991.
ten Ham, M. 2003. Health risks of counterfeit pharmaceuticals. Drug Safety 26:991–7.
Tenover, F. C., and J. E. McGowan Jr. 1996. Reasons for the emergence of antibiotic resistance. The American Journal of the Medical Sciences 311:9–16.
The Medical Letter. 2009. Drugs for MRSA with reduced susceptibility to vancomycin. The Medical Letter 51:36.
US Government Accountability Office. 2011. Antibiotic Resistance: Data Gaps Will Remain Despite HHS Taking Steps to Improve Monitoring. Report to the Committee on Agriculture, House of Representatives. Washington, DC. GAO-11-406.
van Eijk, A. M., and D. J. Terlouw. 2011. Azithromycin for treating uncomplicated malaria. Cochrane Database of Systematic Reviews February 16:CD0006688.
Walsh T. R., and M.A. Toleman. 2011. The emergence of pan-resistant Gram-negative pathogens merits a rapid global political response. Journal of Antimicrobial Chemotherapy [e-pub ahead of print].
Walsh, T. R., J. Weeks, D. M. Livermore, and M. A. Toleman. 2011. Dissemination of NDM-1 positive bacteria in the New Delhi environment and its implications for human health: an environmental point prevalence study. The Lancet Infectious Diseases 11:355–62.
|
|
Wang, C. Y., V. C. Wu, Y. M. Chen, C. T. Su, K. D. Wu, and P. R. Hsueh. 2009. Nasal carriage of methicillin-resistant Staphylococcus aureus among patients with end-stage renal disease. Infection Control and Hospital Epidemiology 30:93–4.
Weber, D. J., W. A. Rutala, M. B. Miller, K. Huslage, and E. Sickbert-Bennett. 2010. Role of hospital surfaces in the transmission of emerging health care-associated pathogens: norovirus, Clostridium difficile, and Acinetobacter species. American Journal of Infection Control 38(5 suppl 1):S25–33.
Weinstein, R. A. 1991. Epidemiology and control of nosocomial infections in adult intensive care units. The American Journal of Medicine 91(3B):S179–84.
Weintrob, A. C., M. P. Roediger, M. Barber, et al. 2010. Natural history of colonization with gram-negative multidrug-resistant organisms among hospitalized patients. Infection Control and Hospital Epidemiology 31:330–7.
Wensing, A. M., D. A. van de Vijver, G. Angarano, et al. 2005. Prevalence of drug-resistant HIV-1 variants in untreated individuals in Europe: implications for clinical management. The Journal of Infectious Diseases 192:958–66.
Whitby, M., M. L. McLaws, and G. Berry. 2001. Risk of death from methicillin-resistant Staphylococcus aureus bacteraemia: a meta-analysis. The Medical Journal of Australia 175:264–7.
White, A. S., R. D. Godard, C. Belling, V. Kasza, and R. L. Beach. 2010. Beverages obtained from fountain machines in the U.S. contain microorganisms, including coliform bacteria. International Journal of Food Microbiology 137:61–6.
Williams, G., and J. C. Craig. 2011. Long-term antibiotics for preventing recurrent urinary tract infection in children. Cochrane Database of Systematic Reviews March 16:CD001534.
Wondemagegnehu, E., and Essential Drugs and Other Medicines. 1999. Counterfeit and Substandard Drugs in Myanmar and Viet Nam: Report of a Sudy Carried out in Cooperation With the Governments of Myanmar and Viet Nam. World Health Organization. http://apps.who.int/medicinedocs/pdf/s2276e/s2276e.pdf.
World Health Organization. 2011. Global Alert and Response (GAR). http://www.who.int/csr/en.
World Health Organization, UNAIDS. 2010. AIDS epidemic. Joint United Nations Programme on HIV/AIDS and World Health Organization. http://data.unaids.org/pub.
Wright, A., and M. Zignol. 2008. Anti-tuberculosis Drug Resistance in the World: Fourth Global Report. World Health Organization. http://whqlibdoc.who.int/hq/2008/WHO_HTM_TB_2008.394_eng.pdf.
Xiong, Y. Q., V. G. Fowler, M. R. Yeaman, F. Perdreau-Remington, B. N. Kreiswirth, and A. S. Bayer. 2009. Phenotypic and genotypic characteristics of persistent methicillin-resistant Staphylococcus aureus bacteremia in vitro and in an experimental endocarditis model. The Journal of Infectious Diseases 199:201–8.
|
|
SECTION THREE: Control and Prevention of AMDR Best Practices
Arnold, S. R., and S. E. Straus. 2005. Interventions to improve antibiotic prescribing practices in ambulatory care. Cochrane Database of Systematic Reviews October 19:CD003539.
Behta, M., B. Ross, and R. Chaudhry. 2008. A comprehensive decision support system for the identification, monitoring and management of patients with multi-drug resistant organisms (MDRO). AMIA Annual Symposium Proceedings 6:1218.
Boucher, H. W., G. H. Talbot, J. S. Bradley, et al. 2009. Bad bugs, no drugs: No ESKAPE! An update from the Infectious Diseases Society of America. Clinical Infectious Diseases 48:1–12.
Cassell, G. H., and J. Mekalanos. 2001. Development of antimicrobial agents in the era of new and reemerging infectious diseases and increasing antibiotic resistance. Journal of the American Medical Association 285:601–5.
Conly, J. 2002. Antimicrobial resistance in Canada. Canadian Medical Association Journal 167:885–91.
Cooper, B. S., S. P. Stone, C. C. Kibbler, et al. 2004. Isolation measures in the hospital management of methicillin-resistant Staphylococcus aureus (MRSA): systematic review of the literature. BMJ 329:533.
Dellit, T. H., R. C. Owens, J. C. McGowan Jr, et al. 2007. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clinical Infectious Diseases 44:159–77.
de Martel, C., and S. Franceschi. 2009. Infections and cancer: established associations and new hypotheses. Critical Reviews in Oncology/Hematology 70:183–94.
Fishman, N. 2006. Antimicrobial stewardship. The American Journal of Medicine 119(6 suppl 1):S53–61, discussion S62–70.
Garrett, L. 2001. The return of infectious disease. In Plagues and Politics, ed. A. T. Smith-Price, 183–194. New York: Palgrave Publishers Ltd.
Goldmann, D. 2006. System failure versus personal accountability--the case for clean hands. The New England Journal of Medicine 355:121–3.
Gonzales, R., K. K. Corbett, S. Wong, et al. 2008. “Get Smart Colorado”: impact of a mass media campaign to improve community antibiotic use. Medical Care 60:597–605.
Guidos, R.J. 2011. Combating antimicrobial resistance: policy recommendations to save lives. Clinical Infectious Diseases 52(suppl 5):S397–428.
Harris, S. R., E. J. Feil, M. T. Holden, et al. 2010. Evolution of MRSA during hospital transmission and intercontinental spread. Science 327:469–74.
Harrison, P.F., and J. Lederberg, eds. 1998. Antimicrobial Resistance: Issues and Options. Workshop Report. Institute of Medicine. Washington, DC: National Academy Press. http://www.iom.edu/Reports/1998/Antimicrobial-Resistance-Issues-and-Options.aspx.
Hemo B., N. H. Shamir-Shtein, B. G. Silverman, et al. 2009. Can nationwide media campaign affect antibiotic use? The American Journal of Managed Care 15:529–34.
|
|
Institute of Medicine. 2002. Linking infectious agents and chronic diseases: defining the relationship, enhancing the research, and mitigating the effects. Forum on microbial threats. http://www.iom.edu/Activities/PublicHealth/MicrobialThreats/2002-OCT-21.aspx.
Jarvis, W. R. 1994. Handwashing--the Semmelweis lesson forgotten? Lancet 344:1311–2.
Knowles, S. M. 2010. Intellectual property. Fixing the legal framework for pharmaceutical research. Science 327:1083–4.
Lateef, A. 2004. The microbiology of pharmaceutical effluent and its public health implications. World Journal of Microbiology & Biotechnology 20:167–71.
Liu, C., A. Bayer, S. E. Cosgrove, et al. 2011. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clinical Infectious Diseases 52:285–92.
Livermore, D. M. 2003. Bacterial resistance: origins, epidemiology, and impact. Clinical Infectious Diseases 36(suppl 1):S11–23.
Michels, H. T., J. O. Noyce, and C. W. Keevil. 2009. Effects of temperature and humidity on the efficacy of methicillin-resistant Staphylococcus aureus challenged antimicrobial materials containing silver and copper. Letters in Applied Microbiology 49:191–5.
Monnet D. L., and K. G. Kristinsson. 2008. Turning the tide of antimicrobial resistance: Europe shows the way. Eurosurveillance 13:19039.
Naber, C. K. 2009. Staphylococcus aureus bacteremia: epidemiology, pathophysiology, and management strategies. Clinical Infectious Diseases 48(suppl 4): S231–7.
Naddeo, V., S. Meriç, D. Kassinos, V. Belgiorno, and M. Guida. 2009. Fate of pharmaceuticals in contaminated urban wastewater effluent under ultrasonic irradiation. Water Research 43:4019–27.
Paskovaty, A., J. M. Pflomm, N. Myke, and S. K. Seo. 2005. A multidisciplinary approach to antimicrobial stewardship: evolution into the 21st century. International Journal of Antimicrobial Agents 25:1–10.
Podolsky, S. H. 2005. The changing fate of pneumonia as a public health concern in 20th-century America and beyond. American Journal of Public Health 95:2144–54.
Pope, S. D., T. H. Dellit, R. C. Owens, T. M. Hooton, Infectious Diseases Society of America, and Society for Healthcare Epidemiology of America. 2009. Results of survey on implementation of Infectious Diseases Society of America and Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Infection Control and Hospital Epidemiology 30:97–8.
Philipson, T., and R. A. Posner. Private Choices and Public Health: The AIDS Epidemic in an Economic Perspective. Cambridge: Havard University Press, 1993.
Phillips, M., and P. A. Phillips-Howard. 1996. Economic implications of resistance to antimalarial drugs. Pharmacoeconomics 10:225–38.
Rybak, M., B. Lomaestro, J. C. Rotschafer, et al. 2009. Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. American Journal of Health-System Pharmacy 66:82–98.
|
|
Schlaes, D. M., D. N. Gerding, J. F. John Jr, et al. 1997. Society for Healthcare Epidemiology of America and Infectious Diseases Society of America Joint Committee on the Prevention of Antimicrobial Resistance: guidelines for the prevention of antimicrobial resistance in hospitals. Clinical Infectious Diseases 25:584–99.
Siegel J. D., E. Rhinehart, M. Jackson, L. Chiarello, and the Healthcare Infection Control Practices Advisory Committee. 2006. Management of Multidrug-Resistant Organisms in Healthcare Settings, 2006. Atlanta, GA: Centers for Disease Control and Prevention.
Small, P. M., and P. I. Fujiwara. 2001. Management of tuberculosis in the United States. The New England Journal of Medicine 345:189–200.
Smith, P. W., G. Bennett , S. Bradley, et al. 2008. SHEA/APIC guideline: infection prevention and control in the long-term care facility. Infection Control and Hospital Epidemiology 29:785–814.
Smith, R. D., and J. Coast. 2002. Antimicrobial resistance: a global response. Bulletin of the World Health Organization 80:126–33.
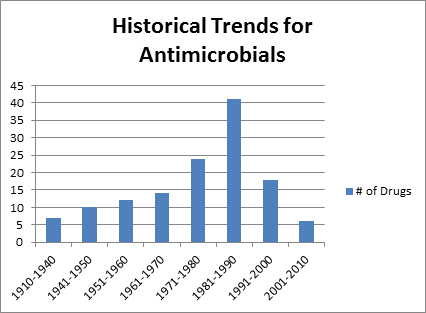
Spellberg, B., J. H. Powers, E. P. Brass, et al. 2004. Trends in antibiotic drug development: implications for the future. Clinical Infectious Diseases 38:1279–86.
Tasina, E., A. B. Haidich, S. Kokkali, and M. Arvanitidou. 2011. Efficacy and safety of tigecycline for the treatment of infectious diseases: a meta-analysis. The Lancet Infectious Diseases July 22 [epub ahead of print].
Tenover, F. C. 2006. Mechanisms of antimicrobial resistance in bacteria. The American Journal of Medicine 119(6 suppl 1):S3–10, discussion S62–70.
US Congress, Office of Technology Assessment. 1995. Impacts of Antibiotic-Resistant Bacteria. U.S. Congress (OTA-H-629). Washington, DC: US Government Printing Office.
Weber S. G., S. S. Huang, S. Oriola,et al. 2007. Legislative mandates for use of active surveillance cultures to screen for methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci: position statement from the Joint SHEA and APIC Task Force. SHEA/APIC position statement.
Weiss K., R. Blais, A. Fortin, S. Lantin, and M. Gaudet. 2011. Impact of a multipronged education strategy on antibiotic prescribing in Quebec, Canada. Clinical Infectious Diseases In press.
World Health Organization. 2005. Containing Antimicrobial Resistance. WHO Policy and Perspectives on Medicines. http://www.who.int/management/anmicrobialresistance.pdf.
Yahav, D., A. Lador, M. Paul, and L. Leibovici. 2011. Efficacy and safety of tigecycline: a systematic review and meta-analysis. The Journal of Antimicrobial Chemotherapy 66:1963–71.
Yeung, W. C., W. D. Rawlinson, and M. E. Craig. 2011. Enterovirus infection and type 1 diabetes mellitus: systematic review and meta-analysis of observational molecular studies. BMJ 342:d35.
|
|
SECTION FOUR: Conclusions
Centers for Disease Control and Prevention. 2010. Facts about antibiotic resistance. http://www.cdc.gov/getsmart/antibiotic-use/fast-facts.html.
Howard, D. H., R. D. Scott 2nd, R. Packard, and D. Jones. 2003. The global impact of drug resistance. Clinical Infectious Diseases 36(suppl 1):S4–10.
Interagency Task Force on Antimicrobial Resistance. 2001. A Public Health Action Plan to Combat Antimicrobial Resistance. Part I: Domestic Issues. http://www.cdc.gov/drugresistance/actionplan/aractionplan.pdf.
Pagani, L., I. C. Gyssens, B. Huttner, D. Nathwani, and S. Harbarth. 2009. Navigating the web in search of resources on antimicrobial stewardship in health care institutions. Clinical Infectious Diseases 48:626–32.
Smith, R.D., and J. Coast. 2002. Antimicrobial resistance: a global response. Bulletin of the World Health Organization 80:126–33.
Teuber M. 1999. Spread of antibiotic resistance with food-borne pathogens. Cellular and Molecular Life Sciences 56:755–63.
World Health Organization. 2005. Containing Antimicrobial Resistance. WHO Policy and Perspectives on Medicines. http://www.who.int/management/anmicrobialresistance.pdf.
|
|