f. Malaria
|
|
In tropical regions, malaria coexists with tuberculosis and HIV/AIDS infections. The dual infection of HIV and malaria contributes to the spread of both diseases in sub-Saharan African (Abu-Raddad et al. 2006) and could result in nosocomial infections and AMDR. A decade ago, the US National Intelligence Council reported that first-line drug treatment for malaria was no longer effective in 80 of the 92 countries where the disease is a major health problem (Gordon and Gannon 2000). The resistance to chloroquine is so widespread that it is currently not recommended as a therapeutic intervention (Adjuik et al. 2004).
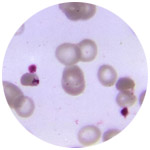
Malaria is a threat to half of the world's population and the cause of death of more than 1 million people annually. Malaria is caused by 4 different protozoan intracellular parasite species transmitted primarily by the bite of the female Anopheles mosquito. ·Plasmodium falciparum ·Plasmodium vivax ·Plasmodium ovale ·Plasmodium malariæ An increase in human infections with Plasmodium knowlesi is being observed in Southeast Asia, probably due to human activities and encroachment into the primate habitat (Lee et al. 2011). Malaria is endemic in parts of Asia, Africa, Central and South America, Oceania, and some Caribbean islands. Malaria infections coexist with HIV/AIDS and tuberculosis in several equatorial countries in the African continent and contribute to the excess burden of morbidity and mortality in the area. According to the WHO, resistance of P falciparum to choloroquine, the cheapest and the most prescribed antimalarial drug, is spreading throughout the endemic countries. Resistance to the combination of sulfadoxine-pyrimethamine that is present in South America and in Southeast Asia is now emerging in East Africa (World Health Organization 2011).
Resistance develops most rapidly with subtherapeutic concentrations of antimalarial drugs. Emergence of resistance to antimalarial drugs is associated with:
-
Greater exposure
-
Use of single, shorter-action conventional drugs first
-
Use of primary antimalarial drugs for nonmalarial indications in high-risk areas (eg, chloroquine for rheumatoid arthritis in a malarial endemic area)
-
Poor compliance with therapy and other preventive measures, such as bed netting at night
-
Failure of monitoring for resistance to prevent spread
-
Lack of clear policy and protocols for use of newer antimalarial drugs
The WHO recommends considering treating malaria with combination therapy using azithromycin, an antibiotic with weak antimalarial properties. No significant benefit for this practice was identified using the Cochrane Database (van Eijk and Terlouw 2011). Isolated cases of resistance to artemisinin were recently reported and a research into antimalarial vaccines is in progress (Breman 2009; Pongtavornpinyo et al. 2008).
|